Aiming for Complete Remission in Diabetes Patients
Addressing Epigenetic Abnormalities in Bone Marrow and Thymus
Despite the global prevalence of diabetes, a complete cure has not yet been found. Attention has been focused on why diabetes resists treatment, and research has progressed. Recently, abnormalities in Vcam1-positive short-term hematopoietic stem cells (Vcam1+ST-HSC), a part of bone marrow-derived cells (BMDCs), have been identified as a major factor in diabetes complications.
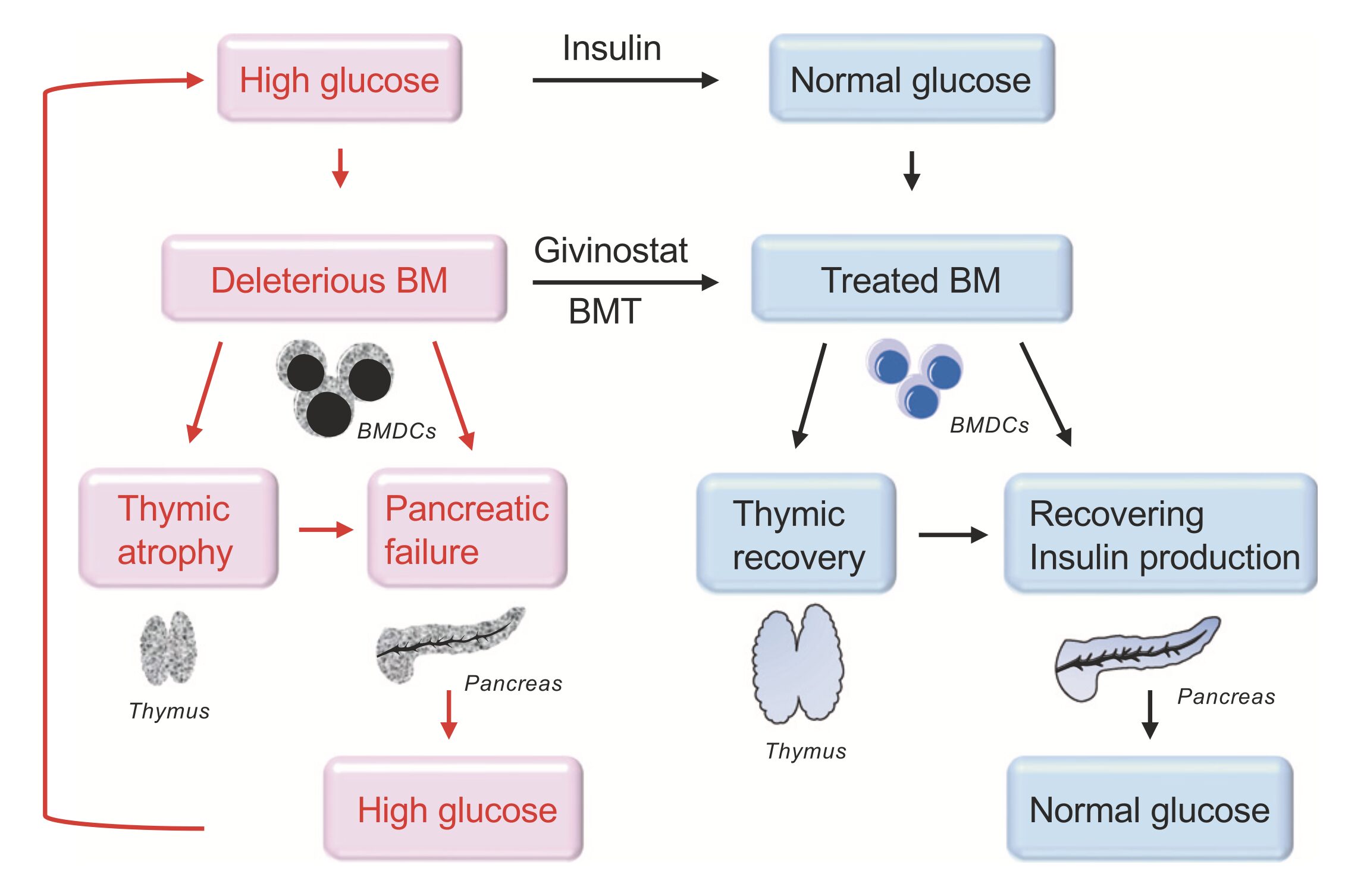
Experiments on diabetic mice investigated whether these abnormal BMDCs continuously damage pancreatic β-cells. Results showed that controlling blood sugar levels with insulin and removing abnormal BMDCs through bone marrow transplantation allowed normal blood sugar levels to be maintained even after stopping insulin therapy.
As an alternative to bone marrow transplantation, abnormal BMDCs showing epigenetic changes were treated with the HDAC inhibitor givinostat. After this treatment, both insulin and givinostat were stopped, yet insulin secretion was maintained, and blood sugar levels remained normal. This combination therapy completely prevented the abnormal BMDCs induced by diabetes from moving to and fusing with cells in the islets or thymus.
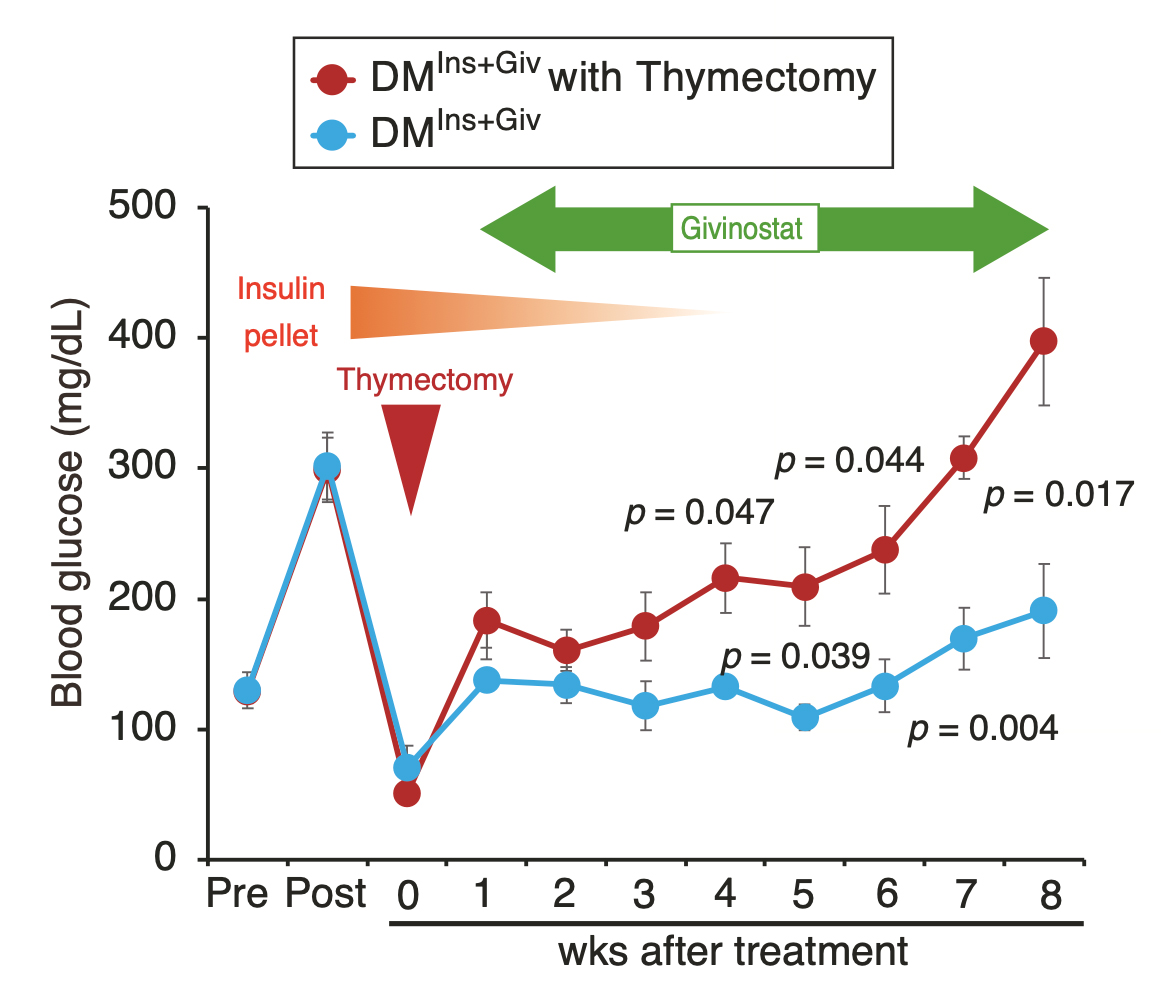
However, the effect of this combination therapy was not observed when the thymus was surgically removed beforehand. This indicates that diabetes involves epigenetic abnormalities in both the bone marrow and the thymus. This combination therapy of insulin and givinostat has potential for clinical application as a new treatment aiming for complete remission in diabetes patients.
Reasons Why Diabetes Is Not Curable
Abnormal Bone Marrow Stem Cells (BMDCs) Inhibiting β-Cell Regeneration
Diabetes is increasing globally, making the development of effective treatments urgent. The focus of our research is on why diabetes is not curable, particularly the regeneration ability of β-cells. β-cells have the ability to regenerate, actively doing so during the perinatal period, and can regenerate under certain conditions in adults. However, in a diabetic state, this regenerative ability is likely reduced.
We discovered that abnormal bone marrow stem cells (BMDCs) play a crucial role in the progression of diabetes. These abnormal cells are generated in a hyperglycemic state and cannot be eliminated by insulin treatment. These cells are believed to destroy normal tissue function and hinder the healing of diabetes.
We hypothesized that treating abnormal BMDCs inhibiting β-cell regeneration in diabetes conditions would restore β-cell regenerative ability and normalize insulin secretion. This hypothesis was tested using STZ-induced diabetic model mice. First, hyperglycemia was controlled with insulin to suppress the generation of abnormal BMDCs. Then, HDAC inhibitors were used to correct the epigenetic changes in these abnormal BMDCs.
This study suggests that treating abnormal BMDCs can enable β-cell regeneration, leading to a potential cure (or complete remission) for diabetes. Additionally, thymus function recovery is expected. These findings open new avenues for diabetes treatment.
Insulin and Histone Deacetylase (HDAC) Inhibitors
A New Approach to Diabetes Treatment
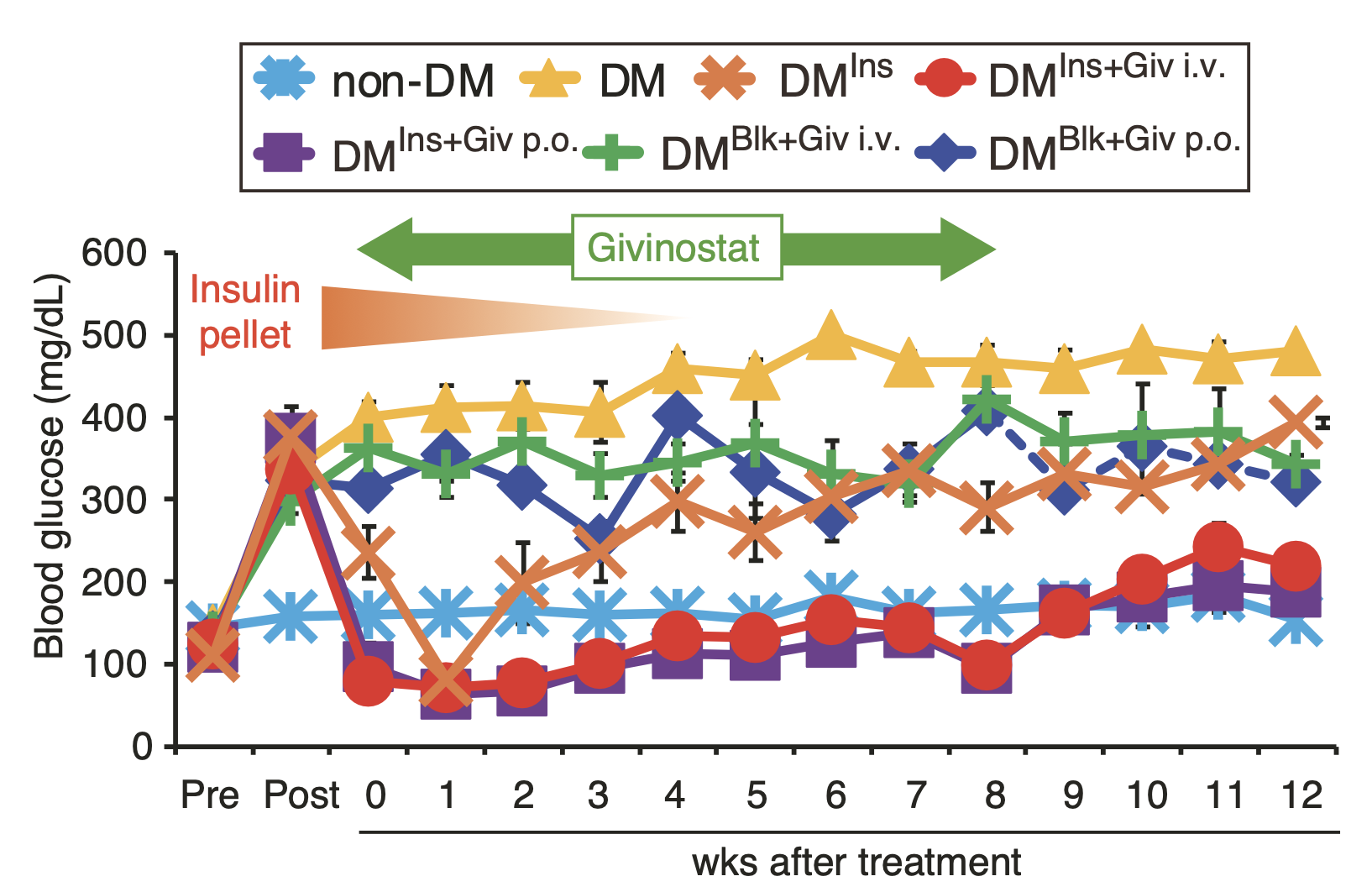
Introducing the latest research findings on diabetes treatment. This study investigated whether the combination of insulin and the histone deacetylase (HDAC) inhibitor givinostat could induce complete remission of diabetes using diabetic mice.
First, epigenetic changes in hematopoietic stem cells in the bone marrow were confirmed to be caused by diabetes. Then, diabetic mice with implanted insulin pellets were treated with givinostat for eight weeks. The results showed that blood sugar control was maintained, and normal blood sugar levels persisted even after the insulin pellets were removed. Additionally, normal blood sugar levels were sustained for another four weeks after stopping givinostat treatment.
These results indicate that the combination of insulin and HDAC inhibitors may be effective in achieving remission of diabetes.
Discovery and Research of Diabetes Stem Cells
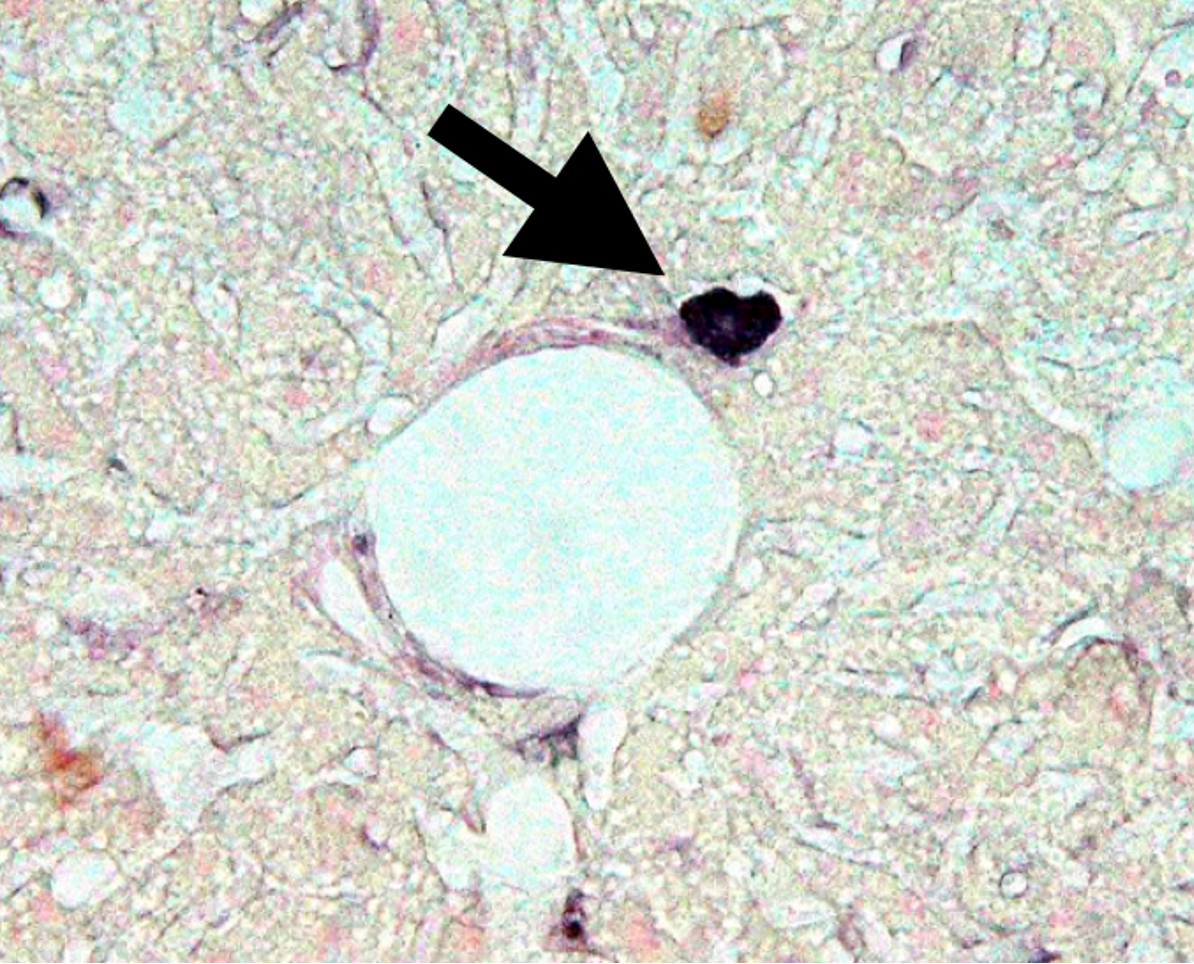
Abnormal cells were found in hematopoietic stem cell fractions that cause diabetes, which do not disappear even when b/s levels are normalized, creating refractory characteristics.
Discovered that diabetes is a disease caused by abnormalities in hematopoietic stem cells and developed a method to cure diabetes by isolating and eliminating “Diabetes Stem Cells.”
Cell Targeting Technology (Biozipcode)
Aiming to develop cell-targeted drugs as a new drug delivery method for the next generation, beyond the current era of molecular-targeted drugs.
Developing a completely new diabetes and diabetes complication cure using Biozipcode that causes no side effects.
Using cell targeting technology with Biozipcode to develop side-effect-free anticancer drugs, providing treatments that minimize patient burden.
Aiming to develop scaffold materials that promote natural wound healing, adhering to tissues without the need for transplantation or suturing, and enhancing quality of life (QOL).
Are You Interested in Research at the Department of Regenerative Medicine?
Are You Interested in Research at the Department of Regenerative Medicine?
You can send a direct inquiry to the Department of Regenerative Medicine through the contact form.